Morning stiffness that turns getting out of bed into an effort. Popping and painful knees that make every step a trial. Fingers that struggle to bend to grasp a coffee cup. We often attribute these symptoms to "wear and tear" or simply getting older, but the real culprit is often arthritis – a complex condition with over 100 varieties that affects millions of people, including the young.
This is much more than just "joint pain." Arthritis can take away our ability to perform our favorite activities and fundamentally disrupt our quality of life. Understanding its forms, causes, and especially its management strategies is the first and most crucial step toward regaining control and movement.
In this comprehensive guide from Adapt.BG, we will delve deep into the world of arthritis – from the anatomy of pain to modern approaches for a better, more active life.
The Anatomy of Pain: What is a Joint and Why Does It Get Inflamed?
 To understand arthritis, we must first understand our joints. They are amazing engineering feats that allow for movement. Every joint consists of several key components:
To understand arthritis, we must first understand our joints. They are amazing engineering feats that allow for movement. Every joint consists of several key components:
- Cartilage: A smooth, elastic tissue that covers the ends of bones, allowing them to glide past each other with minimal friction.
- Synovial Membrane: A thin lining that produces synovial fluid.
- Synovial Fluid: The joint's "lubricant," which nourishes the cartilage and facilitates movement.
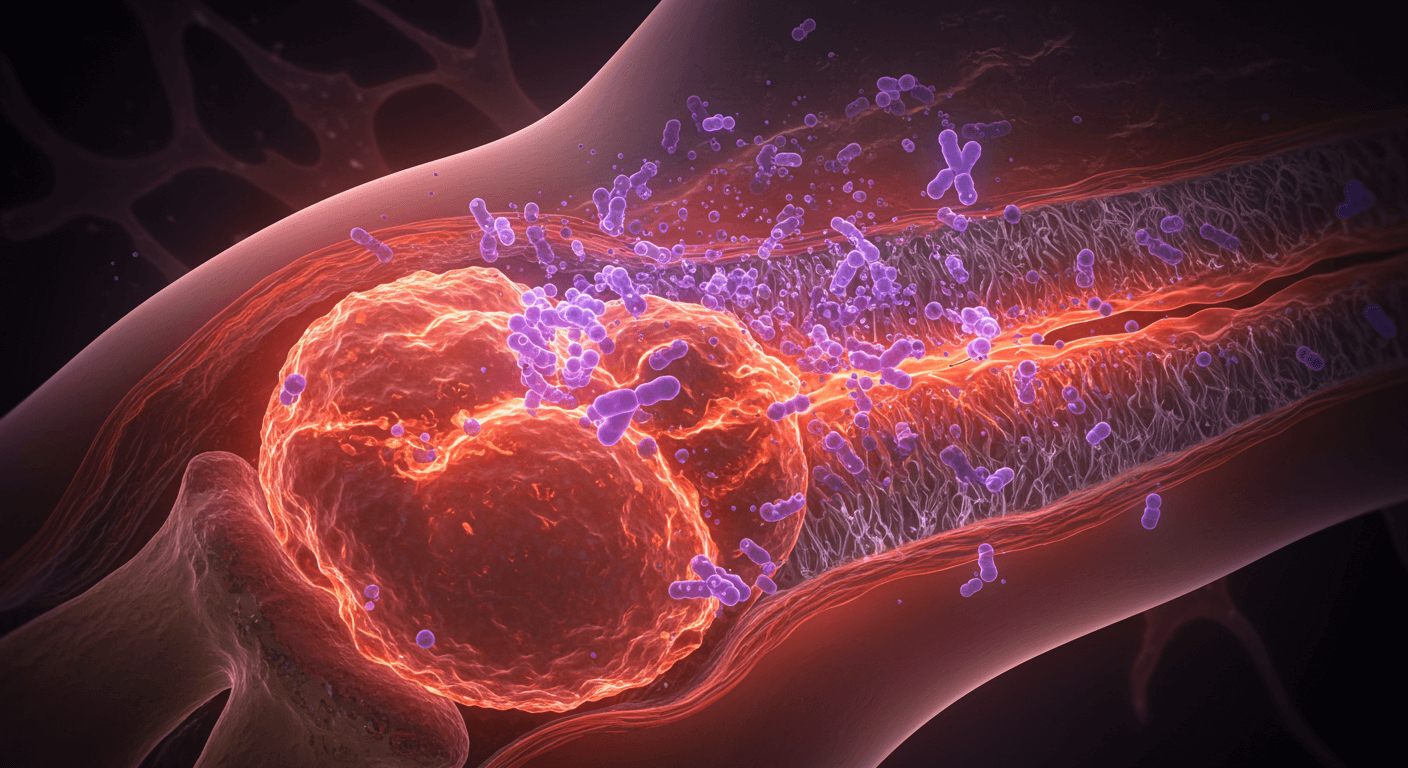
Arthritis (from Greek: arthron – "joint" and -itis – "inflammation") literally means inflammation of the joint. This inflammatory process attacks the delicate balance within the joint, leading to:
- Cartilage Breakdown: The protective layer wears away, causing bone to rub against bone.
- Inflammation of the Synovial Membrane: It swells and produces excess fluid, causing swelling.
- Pain, Stiffness, and Loss of Function: The result of these processes is what we feel as arthritis.

Osteoarthritis vs. Rheumatoid Arthritis: Not All Arthritis is the Same
Although there are over 100 types, two are the most common, yet they have fundamentally different natures:
- Osteoarthritis: The most common form, often called "wear-and-tear arthritis." In this type, the cartilage breaks down over time due to mechanical stress, age, or injuries. It primarily affects weight-bearing joints (knees, hips) and usually appears asymmetrically (e.g., in only one knee).
- Rheumatoid Arthritis: This is an autoimmune disease. The immune system mistakenly attacks its own tissues (the synovial membrane), causing chronic inflammation that can lead to severe joint deformity. It typically affects small joints symmetrically (hands, wrists, feet) and is accompanied by systemic symptoms like fatigue and fever.
Recognizing the Main Symptoms
Symptoms vary depending on the type of arthritis, but there are several common signals to watch for:
- Joint Pain: Can be constant or intermittent (flares). It may feel dull, throbbing, or sharp and piercing.
- Stiffness: Most characteristic is morning stiffness that lasts more than 30 minutes, especially with rheumatoid arthritis.
- Joint Swelling: Visible swelling caused by the accumulation of fluid.
- Redness and Warmth: The skin over the affected joint may be warm and red to the touch, a sign of active inflammation.
- Decreased Range of Motion: Difficulty performing full movements, such as bending a knee or making a fist.
- "Popping" or "Grinding" (Crepitus): A sensation of friction in the joint during movement.
- Systemic Symptoms (especially with RA): Fatigue, weakness, loss of appetite, low-grade fever.
Diagnosis
An accurate diagnosis is crucial, as the treatment for different types of arthritis varies. Your primary care physician or a rheumatologist will take the following steps:
- Medical History and Physical Exam: The doctor will ask about your symptoms and examine your joints for swelling, tenderness, and range of motion.
- Blood Tests: These can detect markers of inflammation (ESR, CRP) or specific antibodies (rheumatoid factor, anti-CCP) that are characteristic of rheumatoid arthritis.
- Imaging Tests: An X-ray can show cartilage loss and bone changes. MRI and ultrasound provide a better picture of soft tissues like the synovial membrane, tendons, and fluids.

Managing Arthritis: Strategies for a Better Life
While there is no cure for most types of arthritis, highly effective strategies exist to manage symptoms, slow progression, and improve quality of life.
Step 1: The Foundations of Good Management
- Movement is Medicine: The most important step. Regular, low-impact exercises (swimming, water aerobics, cycling, tai chi) lubricate the joints, strengthen surrounding muscles, and reduce pain.
- Weight Management: Every pound lost reduces the load on the knees and hips several times over.
- Heat and Cold Therapy: Warm compresses and baths relax muscles and relieve stiffness. Cold compresses (ice) reduce swelling and acute inflammation.
- Balanced Diet: An anti-inflammatory diet rich in omega-3 fatty acids (fish), antioxidants (fruits, vegetables), and fiber can help.
- Daily Living Aids: Using specialized assistive devices can drastically reduce stress on the joints. This includes canes, walkers, sock aids, jar openers, and grab bars for the bathroom.
Step 2: Over-the-Counter Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen and diclofenac reduce both pain and inflammation. They are available over-the-counter and as topical gels.
- Analgesics: Paracetamol helps control pain but has no anti-inflammatory effect.
Step 3: Disease-Modifying Drugs
- Corticosteroids: Powerful anti-inflammatory drugs that are taken orally or injected directly into a joint for rapid relief.
- Disease-Modifying Antirheumatic Drugs (DMARDs) and Biologics: This is the gold standard for rheumatoid arthritis. These medications not only relieve symptoms but also suppress the immune system to slow or stop joint destruction.
When is Surgical Treatment Necessary?
When joint damage is severe and conservative methods fail, surgery may be considered. The most common procedure is arthroplasty (joint replacement), where the damaged joint (most often the hip or knee) is replaced with an artificial prosthesis. This can dramatically reduce pain and restore function.
"Red Flags": When to Seek Immediate Help?
Although arthritis is a chronic condition, some symptoms require immediate medical attention as they can be a sign of a joint infection:
- Sudden, very severe pain and swelling in one joint.
- High fever accompanied by joint pain.
- Intense redness of the skin over the joint, which is hot to the touch.
- Inability to move the affected joint.

Living with arthritis is a marathon, not a sprint. It requires active participation, knowledge, and a partnership with your doctor. With the right management plan combining movement, adequate treatment, and lifestyle changes, you can control your pain, maintain your mobility, and continue to enjoy a full and active life.
The information provided in this article is for educational purposes only and cannot replace professional medical diagnosis or treatment. For health problems, please always consult a qualified physician or rheumatologist.
Grigor Angelov
Date: 26 Aug 2025











Post comment